בית > Reconstructive surgeries > Tear duct bypass/reconstruction surgery

Suffering from constant tearing? Problems with tear drainage can interfere with your quality of life, but the good news is that there are solutions! In this video, Prof. Guy Ben Simon explains tear duct reconstruction – how the problem is diagnosed and what treatments exist depending on age and the severity of the blockage.
Tearing is one of the most common reasons for presenting to an ophthalmologist for oculoplastic surgery. It can be reactive or secondary to dry eye, diseases of the external ocular surface, or eye infections. In these cases, the tearing will be intermittent – appearing occasionally and not constant. It can also be related to exposure to wind or air conditioning. The second cause of tearing is a disruption in drainage as a result of improper eyelid position (ectropion / entropion / retraction) or blockage of the tear ducts throughout their length (eyelid, lacrimal sac and tear drainage tube in the nose). In these cases, the tearing is constant and usually does not depend on external factors.
Tear duct obstruction is one of the most common causes of tearing in newborns and adults (see Congenital Tear Duct Obstruction). It occurs more often in women than in men, and can be on one or both sides.
Complete blockage of the tear duct causes constant tearing, regardless of the weather/exposure to air conditioning or wind. Tears can accumulate in the eye or flow constantly onto the cheek, as well as causing interference with reading and near and far vision. In some cases, acute inflammation of the lacrimal sac appears with redness, swelling around the eye, accompanied by pain and purulent discharge. In other cases, the purulent discharge can be permanent/chronic.

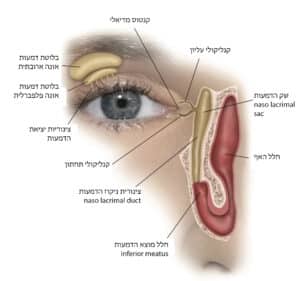
When tears interfere with vision, or constantly run down the cheek and force the patient to wipe their eyes frequently, or when there are recurring eye infections, it is recommended to perform a tear duct reconstruction surgery – Dacryocystorhinostomy. The surgery essentially creates a bypass over the area of obstruction and creates a wider connection between the nasal cavity and the lacrimal sac.
The surgery is suitable for anyone who suffers from a complete blockage of the tear drainage with a constant tear, which mechanically interferes or causes a decrease in vision. In children, the surgery is suitable for those over the age of one and for whom previous procedures such as lacrimal duct irrigation, a balloon or a silicone tube have failed. It is important to understand that in adults with a complete blockage of the tear ducts, the only way is to perform surgery. In children up to one year of age, in many cases the blockage resolves spontaneously or with manual massage of the tear ducts. As well as simpler procedures such as probing, balloon (DCP) or silicone cannula can solve the problem.
The surgery is performed under general anesthesia, and you must come fasting for 6 hours from food and water. If you are taking blood-thinning medications, they must be stopped a certain amount of time before the surgery with the approval of your treating physician. In cases of acute lacrimal sac infections, antibiotics must be taken around the surgery. You must come with a companion to the surgery since you cannot drive after general anesthesia. In most cases, the surgery is outpatient and does not require hospitalization.
As mentioned, the only way to treat a complete blockage of the tear duct is dacryocystorhinostomy (DCR) surgery. During the surgery, the lacrimal sac (located above the blocked duct) is connected to the nasal mucosa through a small window in the bone. There are two approaches to performing the surgery – an external approach (external DCR), through a small incision in the skin, and an endoscopic approach through the nasal cavity without an incision in the skin. In both approaches, when possible, a silicone tube is placed in the tear drainage system for several weeks, in order to increase the chance of success of the surgery. The success rate of both approaches is similar.
In cases where there is an upper obstruction to the tear drainage system (in the delicate drainage canals in the upper and lower eyelids), the surgery will be performed with a permanent glass tube, the Lester Jones Tube, remaining in place. The surgery is performed under local anesthesia with sedation, IV sedation, or general anesthesia. After the surgery, there may be swelling in the eyelid area, as well as a little bloody discharge from the nasal cavity (little leakage in the first few days after the surgery). In external approach surgery, the skin sutures must be removed one to 10 days after the surgery.
In cases where the surgery is performed endoscopically (through the nose) and if there are additional pathologies that may make the surgery difficult (such as a deviated nasal septum leading to obstruction), a combined surgery can be performed with an ENT specialist who will correct the deviated septum before the bypass surgery. Combined surgery is also recommended in the presence of sinus disease or after nasal cavity drainage surgery.
In children, it is common to postpone tear duct bypass surgery only if the last steps, such as irrigation, probing, insertion of a silicone tube or balloon, have not resulted in recovery from the tear. In most cases, surgery in a child, if necessary, will be performed at the age of 4-5 years.
When there is acute inflammation of the lacrimal sac accompanied by redness and pain in the bridge of the nose and around the eyes, antibiotic treatment must first be completed to reduce the inflammation. If possible, bypass surgery can be performed using an endoscopic approach, which leads to complete healing of the obstruction.
In the first few days, slight swelling and subcutaneous hemorrhages may appear in the eyelid area (especially in the external approach) and slight nosebleeds, which pass after a few days. In rare cases, nosebleeds may occur several days after surgery, which requires immediate referral to an ENT doctor (to locate the source of the bleeding). The silicone tube that was placed during surgery is removed after several weeks to months. In cases of a glass tube (when there is an upper obstruction in the tear ducts after surgery, chemical damage/burn) the tube remains permanently in place and is used to transport tears from the eye to the nasal cavity.
It is important to understand that near the time of surgery and in the presence of the silicone tube, tearing may continue, also due to edema and swelling of the nasal mucosa. In most cases, the tearing disappears after a few weeks and sometimes only when the silicone tube is removed. In certain cases where there is no certain diagnosis of complete obstruction, Prof. Ben Simon sends for additional tests such as lacrimal duct mapping – a test that shows the physiological passage of tears.
The clinic usually performs a lavage of the tear ducts using a fine cannula, which can locate the site of the blockage. The clinic has advanced endoscopic equipment that allows for endoscopic evaluation of the nasal cavity, and examines the feasibility of performing the surgery using an endoscopic approach.
It is important to choose an ophthalmologist with a specialization in eyelid surgery – oculoplastics, a unique field that focuses on eyelid, eye socket and tear duct surgery. As well as having experience in tear duct surgery, who will be able to diagnose and adjust the surgery or treatment required for you. If necessary, you can consult with previous patients to gain an understanding of the treatment and recovery.
During the meeting, an initial introduction is made, the patient’s wishes are understood, and expectations are adjusted to the possible outcome. Prof. Ben Simon performs a comprehensive examination of the eye and tear ducts to assess diseases and associated conditions that will require adjustment of the surgery to the health of the eye. After a discussion with the patients, an optimal treatment plan is made and the type of surgery most appropriate for the problem and the patient is selected. After the examination, patients go to the clinic manager to complete tests and receive the technical details of the surgery, including scheduling an appointment. The clinic team includes Miri Sapir, who receives the patient, completes some of the preliminary tests, and serves as an aesthetic consultant, and Anna Kasner, the clinic manager, who coordinates the surgeries and obtains full details about the nature of the process.
In cases of complete blockage of the tear drainage, the only way to treat it is to undergo DCR surgery. This surgery will usually be performed endoscopically through the nasal cavity without a skin incision, or in some cases, with an open approach with a small skin incision in the bridge of the nose. At the end of the surgery, a silicone tube is left through the bypass to increase the chance of success. Prof. Ben Simon removes the tube in the clinic about a month after the surgery.
Surgery is not necessary, but in these cases the symptoms of constant tearing, with or without purulent discharge, and recurrent infections do not go away. In these cases, systemic antibiotic treatment may be necessary to treat the infection.
If the tear duct cannulation is unsuccessful, additional cannulation can be performed with the insertion of a silicone tube or a balloon to dilate the tear ducts (balloon dacryoplasty). If these procedures are unsuccessful and there is still a persistent tear, tear duct reconstruction surgery (DCR) can be performed (see above).
The goal of the surgery, in both techniques, is to bypass the blockage in the tear drainage duct. It is generally better to have the surgery endoscopically, to avoid a skin incision, and to avoid swelling and hemorrhages around the eyes.
However, when there is technical difficulty in performing the surgery using the endoscopic approach due to a deviated septum or a narrow nasal cavity, the surgery can be performed using an external approach or a septum repair can be performed in addition to the bypass surgery.In the latter case, the septum repair is performed at the time of surgery in conjunction with an otolaryngologist. An advantage of the open approach surgery is that it can be performed under local anesthesia with intravenous sedation and there is no need for general anesthesia. In general, both surgeries are excellent with a high success rate (around 90% in the first surgery), and the surgical scar in the open approach is almost imperceptible.